Stature Lengthening
Dr O’Carrigan is currently NOT performing Stature Lengthening Procedures nor assessing patients for that procedure as of January 2022.
The current COVID situation is creating an uncertain and unstable environment that makes continuity of care difficult in both the public and private hospital environment.
Stature Lengthening is a time consuming process that requires careful follow up and the ability to take patients to theatre at short notice to deal with any problems that may arise during the lengthening process and this is currently not possible because of the suspension of elective surgery.
The interruption to elective surgery that has occurred on three occasions in the last two years has created a significant backlog of patients requiring elective surgery to relieve pain and correct deformity and it is these patients that require prioritisation of care and therefore Stature Lengthening Surgery should not be diverting resources away from the care of these patients.
It is also not possible to provide continuity of care for patients outside of Sydney - particularly if they are interstate - the COVID situation creates uncertainty with respect to the availability of flights to be able to attend appointments and care episodes and those flights themselves put the patient at increased risk of contracting COVID-19 and this can have serious consequences.
It is possible to conduct stature lengthening using the Precice nail but the nail is titanium and telescopic and is more liable to fracture than standard non lengthening nails.
The Stryde Nail is a telescopic lengthening nail and it is stainless steel and therefore less prone to mechanical failure than the Precice nail and is preferable for this reason. The Stryde Nail is not currently available for use as it is undergoing further regulatory review.
Once that review process is completed and the nail is available for use then it would be more suitable for stature lengthening procedures than the Precice. It is NOT KNOWN when this process will be completed.
Therefore it is for these reasons that I am not currently assessing patients for stature lengthening or performing those procedures until The COVID situation stabilises and we can confidently predict there will be no further interruptions to elective surgery (unknown timeframe).
The Stryde Nail is available for use(Unknown timeframe)
Dr Tim O’Carrigan MBBS FRACS FAOrthA
Orthopaedic Surgeon
Introduction
What is Stature Lengthening
Stature Lengthening is the surgical lengthening of the femurs or tibias to increase an individuals height.
A patient’s height can become a major source of psychological distress for a patient. Height can affect the way a patient FEELS they are perceived in society and it drives some patients to pursue a surgical solution in stature lengthening. In some patients Stature Lengthening does allow them to move on with greater confidence and overall psychological satisfaction but for people with Body Dysmorphic Disorder then stature lengthening- like all cosmetic surgery - will not alleviate psychological distress and they are unlikely to be satisfied with even a “technically” successful result.
The aim of offering stature lengthening is to help alleviate the psychological distress that patients can feel as a result of their height - most of the time surgeons are trying to alleviate physical pain but in this situation it is to relieve psychological pain.
We cannot offer stature lengthening to patients with BDD and it is an important part of our assessment process including psychological assessment to identify patients with BDD.
Stature Lengthening is achieved using telescopic intramedullary nails and performing surgical fractures of the bone called “osteotomies”. Before these osteotomies heal the nail is lengthened approximately 1mm per day in the femur and a little slower in tibias at 0.75mm per day. The nails contain an internal magnet which is rotated by applying an external magnetic field through a device called an ERC(External Remote Control). The patient is taught how to do this prior to discharge from the hospital. It is a very simple process once understood.
The patient is seen every two weeks during the lengthening process with repeat X-rays and clinical examination to determine that the bone is lengthening at the required rate and that the patient is maintaining good joint range of motion and also to pick up any potential problems that may be developing early so that they can be corrected.
Once out to length the patient is seen on a monthly basis until bone healing is complete.
The nails are removed at a minimum of 12 months once bone healing has matured sufficiently based on xray appearances.
What Stature Lengthening does do
Stature Lengthening simply makes you taller
What Stature Lengthening doesn’t do
Stature Lengthening does not make you smarter, better looking, more athletic or better at your job. All of these benefits are controlled by the patient’s attitude and how they choose to move on with their life after the lengthening process.
In terms of physical prowess it often has the opposite effect. Patients often can’t run or jump as well as they were able to prior to the lengthening. This is because joint range of motion and muscle strength are influenced by the bone and muscle length ratio and when the bone is lengthened the muscles do not lengthen as easily and this often leads to them becoming tighter. This affects joint range of motion and muscle strength negatively. Also prolonged limited weight bearing also can lead to loss of muscle bulk and this also affects strength.
These effects can be reduced over time as the patient rehabilitates but patients often do not return to their original strength and physical activities they were capable of prior to the
lengthening process. So therefore you NEVER do stature lengthening in order to play sport better or be a better athlete.
Process
At the Limb Reconstruction Centre at MQ Health the patient attends the clinic for a consultation with Dr O’Carrigan for an initial assessment and information session. During this consultation a history is taken and physical examination performed plus X-rays conducted and analysed.
A discussion of the reasons why the patient wishes to undergo lengthening as well as their height goals are also canvassed.
A lengthy discussion is undertaken with the patient explaining the limb lengthening process, what it can achieve and what it won’t achieve as well as the potential risks and complications.
The patient is referred to:
- Dr Chris Basten Clinical Psychologist. Chris is very experienced in assessing patients needing to undergo major reconstructive surgeries and a suitable report from Dr Basten is an absolutely mandatory requirement prior to committing to Not all patients that want to undergo stature lengthening are in fact psychologically suitable to undergo this treatment and it is important for the patients benefit to identify this prior to surgical treatment.
- Noelle Coleman RN- Noelle is a Limb Reconstruction Clinical Nurse Consultant who conducts a home assessment and education session with the patient and significant others. Limb Lengthening is a significant undertaking that cannot be completed alone and the patient requires significant practical and emotional support and also needs to be living in an appropriate physical environment to allow for prolonged periods of reduced mobility. Noelle is able to ensure that this is the case and she provides a report to Dr O’Carrigan.
- Dr Tim Ho is our Pain Management Physician and a preoperative consultation with Tim is required to help educate the patient on pain management and to set a pain management plan in place.
- A detailed quote is also provided to the patient so that they are aware of the costs involved which are substantial.
If the requisite reports are satisfactory and the patient is deemed suitable for lengthening and they have received and accepted the quote then the patient is seen in the clinic again and informed consent obtained and a theatre date determined.
Femoral Lengthening
The patient usually undergoes bilateral femoral lengthening first and then tibial lengthening as a separate treatment episode if more lengthening is desired.
A realistic goal for most patients is 5cm in the femur. Some patients can lengthen more if they get to 5cm and are maintaining good joint range of motion, good pain control and their X-rays are satisfactory. 7cm is the upper limit of what is possible. Lengthening will be stopped if the patient is NOT maintaining joint range of motion and they are getting joint contractures.
The surgery involves a general anaesthetic. Indwelling urinary catheter is inserted once the patient is asleep. One side is operated on at a time and after the leg is prepped and draped the osteotomy site is determined using xray and percutaneous drilling performed to “ventilate” the femur. This is to reduce pressure build up in the femur with reaming and reduce the risk of fat embolism.
The medullary canal is entered through the top of the femur and a wire passed down the middle of the bone and reaming is performed. This is the use of sequentially wider cannulated drills to create a path for the nail. We usually ream 1.5 to 2mm wider than the diameter of the nail to ensure easy insertion of the nail and to facilitate lengthening.
A wire is inserted into the top of the femur and the bottom of the femur- they are parallel and we use this marker to ensure that we are maintaining the correct rotation during nail insertion.
The nail is inserted up to the osteotomy site and an osteotome(bone chisel) is used to complete the osteotomy. The nail is inserted across the osteotomy and once fully seated cross locking screws are placed in the top and bottom of the nail. Visual confirmation of maintenance of correct rotation is confirmed with checking the previously placed wires. Wounds are closed in layers and then the surgery is repeated on the other leg.
The patient is taken to recovery and then the ward. They have “patient controlled analgesia” or PCA as well as nurse administered medication for pain control.
As the patient recovers in the following days they are taught by Physio how to mobilise- weight bearing is limited to transfers where a patient goes from the wheelchair to the bed or to the toilet or shower. Most mobility is provided by a wheelchair.
Patients are discharged home once it is clear the surgical wounds are settling and there is good pain control and mobility has been confirmed. Noelle Coleman educates the patient on the lengthening process which requires the application of the ERC(External Remote Control) which is the unit that creates the magnetic field which drives the internal magnet and thus lengthening.
The patient commences lengthening at day 7 postop at 1mm per day and the first postop appointment is at two weeks. This is where stitches are removed and an xray taken to ensure lengthening has commenced.
The patient is seen every two weeks in the clinic with repeat X-rays to ensure the lengthening process is continuing and to check joint range of motion is being maintained and there is adequate analgesia.
5cm lengthening is usually obtained by 2 months postop. At this point lengthening is usually stopped. It can be continued if certain conditions are met and the patient wishes to lengthen more which is usually the case. They must have good pain control, be maintaining joint flexibility and have satisfactory X-rays. Lengthening can continue to a maximum of 7-8cm but will be stopped if any of these conditions are no longer met.
Once the patient is out to length then they are reviewed on a monthly basis with clinical examination and X-rays. As the bone healing progresses then they can mobilise on crutches or a frame and gradually increase their weight bearing.
The usual course of events is lengthening for 2 months. Full weight bearing with or without walking aids by 4 months and fully healed by 6 months. Full recovery takes another 12 months.
Tibial Lengthening
Our approach is to NOT overlap the femoral and tibial lengthening but to treat each lengthening as a completely separate treatment episode.
A patient can only undergo tibial lengthening once they have fully healed from the femoral lengthening. That is bone healing, full range of motion of joints and a normal gait.
The tibial lengthening process is similar to the femoral with some important differences. It is done under a general anaesthetic with insertion of a urinary indwelling catheter.
The fibula is osteotomised through an incision on the side of the leg using drill holes and an osteotome. This wound is closed.
Stabilisation of the proximal and distal tibiofibular joints is performed with insertion of a screw between the top of the fibula and the tibia and the bottom of the fibula and the tibia. With insertion of the top screw care is taken to avoid injury to the common peroneal nerve as it passes around the fibular neck.
This surgery is done to ensure the fibula lengthens with the tibia and there is no adverse affects on the ankle or the knee.
The osteotomy site of the tibia is identified using xray and drill holes placed across is to vent the tibia.
An incision at the top of the tibia is made to allow reaming of the tibia and insertion of the nail. Access is achieved by incising next to the patella tendon and retracting it to the side and then passing a wire down the middle of the bone and progressive reaming prior to insertion of the nail.
The nail is inserted under xray control and the osteotomy is completed and the nail advanced across the osteotomy ensuring rotational control is maintained and once seated the locking screws are inserted across the top and bottom of the nail. Wounds are closed in layers and dressed and then the other side is prepped and draped and the same surgery performed on the other side.
Postoperatively the patient starts lengthening at 10 days and the lengthening is 0.75mm per day. It is slightly slower with the tibia compared to the femur.
The patient is reviewed every two weeks with X-rays and clinical examination and it takes 12 weeks to achieve 5cm of lengthening.
Ankle flexibility must be maintained to continue lengthening. There is a tendency to achilles tendon contracture and if this occurs then achilles lengthening may be necessary.
Patient would normally be full weight bearing by 5 months and be fully healed by 7-8 months.
Blocking Screws
These are screws that are inserted next to the nail in order to guide the nail position and prevent secondary deformity occurring with lengthening.
Unscheduled Surgery
All the planned procedures are identified to the patient during the consent process. Patients are closely monitored during the lengthening process and if a problem occurs it may require surgical intervention to correct. Therefore the patient needs to understand that they may require unscheduled surgery. It is important to identify problems early and treat them aggressively. This may take the form of extra physiotherapy or slower lengthening rates but may involve surgery.
Pain and Stature Lengthening
Stature Lengthening unfortunately is not a pain free process and there can be substantial pain involved.
There is the early postoperative pain but this tends to settle relatively quickly. The early lengthening often involves little pain but the pain peaks towards the end of lengthening when the soft tissues are at their maximum tension.
Once length has been achieved and the lengthening stopped then the pain tends to settle relatively quickly and this is accelerated by bone healing progression.
All steps are taken to try to ensure good pain management under the guidance of Dr Tim Ho and liason with Noelle Coleman.
Work and Stature Lengthening
Work in any form is usually not possible when the patient is lengthening. This is because of pain and pain medication and reduced mobility one cannot commit to reliably providing a service.
Once lengthening has been completed then patients are often able to return to office work from home. COVID has made this process a lot more common place.
Heavy manual labour and site visits cant begin until the patient has healed adequately which means a substantial time off work of up to 6 months.
Nail Removal
The femoral and tibial nails can be removed after a minimum of 12 months if X-rays show that there is adequate bone healing and remodelling. This is done under a general anaesthetic and would usually involve bilateral femoral nail removal then bilateral tibial nail removal
Complications
General Anaesthetics
Stature Lengthening obviously requires general anaesthesia and whilst anaesthesia has become a very safe procedure with advances in medications, monitoring equipment and training there are inherent risks and in rare circumstances they can be life threatening. In rare circumstances one can die under an anaesthetic or have a major medical event such as a heart attack or stroke.
Infection
Deep infection is a rare complication but it can occur and it is extremely serious if it does.
This requires removal of the lengthening nail and extensive debridement to remove the infected tissue then insertion of an antibiotic impregnated nail- this is a rod or nail coated with antibiotic impregnated cement which is inserted into the medullary canal. This obliterates dead space and the antibiotics leak out of the cement to provide high local concentrations of antibiotics.
In the femur the nail is locked and in the tibia it is often supplemented with an external fixateur to provide stability.
Tissue samples are sent to the lab to identify the organism and its sensitivities and the appropriate IV antibiotics given for up to six weeks depending on the organism and the advice from the infectious diseases specialist.
Once the infection is eradicated- this is judged on xray appearances, blood tests(ESR, CRP) and the clinical findings then the antibiotic nail is removed and replaced with a definitive nail.
DVT Pulmonary Embolism
DVT is Deep Venous Thrombosis and this can complicate any surgery. DVT’s can enlarge and become unstable and break off and travel to the lungs- this is called Pulmonary Embolism and if the clot is large enough it can lead to cardiac arrest and sudden death.
DVT’s are diagnosed by Doppler Ultrasound and once identified can be treated with anticoagulants. This is usually in the form of a tablet.
DVT’s are prevented by a number of steps taken in theatre such as calf compressors and early mobilisation. Patients are often given injections called clexane. They are often sent home on aspirin.
Nerve Injury
Nerve injury with femoral lengthening is extremely rare because the nerves at risk(femoral and sciatic nerves) are both in front of and behind the femur and well away from the surgical incisions.
In the tibia there are nerves at risk.
The Saphenous nerve passes down the inside of the knee and it has branches that pass across the front of the knee called the “Infrapatellar” branches. These branches are too small to be seen and cant be avoided so it is common to have some numbness around the lateral aspect of the knee after tibial nail insertion. This numbness does not affect the muscles that move the knee but can contribute to altered feeling with kneeling. It can resolve but may not completely resolve.
The nerve of most concern is the Common Peroneal Nerve. This nerve is a branch of the sciatic nerve and passes across the neck of the fibula on the lateral aspect of the knee. It is an important nerve because it supplies the muscles to the anterior and lateral compartments of the leg and injury to it can lead to Foot Drop which doesnt always resolve.
When we lengthen the tibia we need to insert a screw across the fibula to the tibia at the knee and ankle level to stabilise the fibula to the tibia with lengthening. At the knee level the common peroneal nerve is at risk and extreme care is taken to insert the screw without causing injury to the nerve.
The attached picture is of a common peroneal nerve as it passes over the fibula neck. This surgery was done to release around the Nerve and was not associated with stature lengthening.

Common Peroneal Nerve passing over the fibular neck
Blood Vessel Injury
The femoral artery which supplies the leg passes down the front and inside of the leg so is not seen with insertion of a femoral nail. Injury to the artery is extremely rare but it is possible to injure the artery with the femoral osteotomy or drilling for the locking screws.
In the tibia major blood vessel injury is also rare.
Injury to a major artery can be limb or life threatening. Excessive bleeding can lead to compartment syndrome.
Compartment Syndrome
The muscles of the leg are separated into compartments which are groups of muscles that are surrounded by fascia( fibrous tissue). If you get excessive swelling within a muscle compartment the capillaries can be “squeezed” down which then leads to muscle ischaemia and extreme pain.
Pain is the first and most important sign of compartment syndrome. Some pain is obviously expected from surgery but pain out of proportion to what one would expect is a sign of possible compartment syndrome.
The leg below the knee is most at risk of compartment syndrome.
If compartment syndrome is diagnosed it is a surgical emergency and it needs fasciotomies which is surgery to cut the fascia and allow the muscles to expand restore their blood supply thereby relieving pain.
If compartment syndrome is not diagnosed then it can lead to permanent muscle damage and contractures and amputation in the worse case scenario.
Fat Emobolism
The middle of long bones such as the femur and tibia are called the Medulla. The medulla of long bones are filled with marrow. This marrow has a lot of fatty tissue in it because the bone marrow in long bones do not contribute to making red blood cells. Red Blood Cells are mainly produced by bone marrow in the axial skeleton which is the pelvis, ribs, spine.
When we create the path for the nail we have to ream the medulla- this is a cannulated flexible drill of increasing size that is passed down the bone. In that process we know that fatty material gets into the blood stream and is filtered by the lungs.
In the vast majority of times this has no effect. Rarely it causes an inflammatory response in the lungs which requires oxygen support but tends to resolve quickly over 48-72 hours.
In extremely rare situations this can lead to a widespread systemic uncontrolled inflammatory response which can be life threatening.
Fat Embolism is more common in a trauma situation but can occur with routine elective nail insertion and it is not possible to determine pre-operatively who this might occur to.
Premature Consolidation
The standard rate of lengthening for femurs is 1mm per day and 0.75mm per day for tibias. Occasionally a patient forms regenerate too quickly and stops lengthening. This is called Premature Consolidation.
If this occurs then we need to return to theatre to repeat the osteotomy to allow us to continue lengthening.

Premature consolidation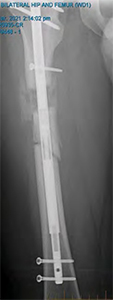
Osteotomy to continue lengthening
Poor Regenerate
The opposite to premature consolidation can occur - this is where the regenerate bone formation is poor and if it remains so then surgical intervention is required.
This takes the form of debridement of the regenerate gap and bone grafting and plate fixation to provide stability across the distraction gap. There is often too much movement

Exchange to a trauma nail with correction of alignment
Poor regenerate formation required bone grafting and plating with eventual
occurring at the distraction gap to allow good bone formation and the plate adds stability. The Precice nail may also be exchanged for a single piece trauma nail.
Nail Fracture
The precice nail is a titanium nail that is telescopic and as a result it is not as strong as a trauma nail which is made of a single piece of solid metal- usually titanium as well.
There are significant bending forces that the nail has to withstand with lengthening and this is exacerbated by weight bearing so therefore weight bearing needs to be restricted until there is evidence of bony bridging across the regenerate.
The precice nail can and does fracture on occasion- this is usually at the junction of the wider and narrower parts of the nail. If this occurs then it requires revision surgery to exchange the nail for a trauma nail and we usually use external fixation in theatre to maintain the correction whilst we exchange the nails.
The Stryde Nail is made of stainless steel and potentially will reduce the incidence of fracture but that is to be determined and the stryde nail is not currently available in Australia.
Malalignment
Malalignment can occur with lengthening as the muscle forces acting on the bone are often asymmetrical

8cm femoral lengthening with nail fracture and varus malalignment
There is a tendency to go into valgus in the tibia as a result of the soft tissue forces and if this occurs it may need surgery to correct. The femur can go into valgus or varus depending on the net soft tissue and mechanical forces.
This is usually an exchange nailing to a trauma nail with external fixation which allows us to remove the precice nail and correct the malalignment then insert the trauma nail in the corrected position.
Malrotation
As the nail is inserted the bone is cut(osteotomy) - the nail is advanced across the osteotomy and then locked proximally and distally to provide stability. In the interval between osteotomy and locking the nail it can be extremely easy for the bone to internally or externally rotate creating a “malrotation”.
If this does occur then it requires revision surgery to correct.
We take a number of steps in theatre to guard against this occurring.

This patient demonstrates a mild external rotation malunion on his right
Joint Contracture
When the bone lengthens the soft tissues also have to lengthen and in the muscles the tendinous part of muscles tend not to stretch and lengthen as easily. This is particularly true of muscles that cross two joints.
In the femur the muscle most at risk is the Tensor Fascia Lata muscle which is attached to the pelvis and then becomes a long fascial band that bypasses the hip joint and the knee joint to attach to the top of the tibia on the lateral side. At the level of the knee it is known as the ITB or Iliotibial Band.
The femur also has the Rectus Femoris which is part of the quadriceps muscle and this crosses the knee and the hip and the hamstring muscles in the back of the thigh also cross the knee and hip.
With tibial lengthening it is the Gastrocnemius or calf muscle that crosses the knee and the ankle and is most at risk of contracture- this causes an “equinus” contracture where your ankle is stuck pointing down.
The main goal during lengthening is to maintain joint range of motion and flexibility. Patients vary with their diligence in doing exercises and they vary with the genetic makeup in that people vary in their soft tissue flexibility.
If someone starts to develop joint contracture during lengthening then we will slow down the rate of lengthening to see if they can “catch up” and restore the joint range of motion. If this is not occurring then lengthening will stop even if it is short of the patients goal.
Sometimes it is necessary to do surgery to release tight muscles to facilitate the restoration of the full range of motion.
It can be possible to repeat the osteotomy and recommence lengthening at a later date if the patient is able to restore their range of motion and still achieve the original lengthening goal. It is better to do two shorter lengthenings than one long lengthening and be left with a permanent contracture.
Summary
Stature Lengthening can be performed in the femurs and tibias as separate episodes of care. It involves careful preoperative assessment and education to determine if a patient is suitable and ready to undergo lengthening from a psychological, physical and practical (proper supports) level.
Safe lengthening requires realistic goals and close co operation between the treating team and the patient and carers.
The aim of treatment is to achieve the desired length whilst maintaining joint range of motion and avoiding complications.
Dr Tim O’Carrigan
MBBS FRACS FAOrthA
Limb Reconstruction Service New South Wales
Limb Reconstruction Centre at MQ Health
